When your wisdom teeth start to play up, it’s not always obvious what to do. Some people breeze through it, while others cop a world of trouble from the get-go. So how do you know if your wisdom teeth are quietly settling in or setting you up for long-term dental drama? Wisdom tooth extraction isn’t just about relieving pain — it can be a preventative move that heads off more serious problems down the track. From crowding your other teeth to sparking infections, these molars can do more damage than you’d expect. This article examines how a proactive approach to wisdom tooth removal can significantly impact your oral health.
Why do some patients need a wisdom tooth extraction earlier than others?
Some people get an easy run, but others? Not so lucky. The timing of wisdom tooth issues depends on a mix of genetics, jaw space, and how the teeth erupt. Here’s why early extraction might be needed:
- Lack of jaw space: Not everyone’s mouth has room for extra molars, leading to painful crowding early on.
- Impacted eruption: Teeth growing sideways or stuck in the gum line can lead to infections or cysts.
- Recurring gum inflammation: Pericoronitis, or gum swelling around a partially erupted tooth, often flares up repeatedly.
- Orthodontic interference: Emerging wisdom teeth can undo years of orthodontic work by pushing other teeth out of alignment.
It’s no surprise many people in their late teens or early twenties get theirs out. If the signs show early, your dentist might call time before bigger problems crop up.
What dental problems can arise if an impacted wisdom tooth is ignored?
Ignoring an impacted molar can be like ignoring a rattling noise in your car — things can get worse, fast. Here are some of the main issues you might run into:
- Infections and abscesses: Trapped food and bacteria can cause painful gum infections or pus-filled abscesses.
- Decay in nearby teeth: Impacted wisdom teeth often press against second molars, making cleaning tough and decay more likely.
- Cysts and jaw damage: Fluid-filled cysts can form around the impacted tooth, eating into jawbone over time.
- Persistent pain: Nerve pressure or inflammation can cause throbbing that won’t quit without intervention.
It’s worth knowing that the risks of neglecting post-extraction care instructions may also add to the problem, especially if you delay or skip treatment.
How is a surgical tooth extraction different from a standard removal?
Not all extractions are equal — surgical ones are more involved, but sometimes unavoidable. Here’s what makes surgical removals different:
- Gum incision required: If the tooth is under the gum or bone, the dentist needs to cut into the tissue to reach it.
- Tooth sectioning: For tricky angles or hard-to-reach positions, the tooth may need to be cut into pieces before removal.
- Longer healing period: The more complex the procedure, the longer the recovery. Swelling and soreness may hang around for a week or more.
- Specialist referral potential: In some cases, particularly for deeply impacted teeth, a specialist oral surgeon may step in.
Despite sounding intense, surgical removal is often the most efficient path to prevent further damage, especially for wisdom teeth buried deep in the jaw.
Which signs indicate that molar extraction might be necessary?
Don’t ignore these telltale signs — they often mean that wisdom tooth removal is on the cards:
- Persistent jaw or gum pain: Aching or throbbing pain at the back of your mouth can be a red flag.
- Swelling or redness near back molars: These symptoms can mean infection or irritation.
- Bad breath or a foul taste: Often caused by trapped food and bacteria around a partially erupted tooth.
- Visible crowding or shifting teeth: Wisdom teeth pushing against other teeth can gradually misalign your smile.
When these signs crop up, a reliable solution for safe wisdom tooth extraction can often provide lasting relief and prevent further disruption.
Can wisdom tooth extraction reduce the need for future orthodontic work?
Absolutely. Proactive wisdom tooth removal can prevent a lot of issues that might otherwise send you back to the ortho chair. Here’s how:
- Stops teeth from shifting: Impacted or crowded wisdom teeth can push other molars forward.
- Protects orthodontic investment: If you’ve had braces, removal can help maintain your straight smile.
- Prevents bite issues: Avoid developing malocclusions or uneven wear due to pressure from wisdom molars.
- Reduces jaw tension: Less crowding means less pressure on the jaw and muscles over time.
Removing molars early is tied to the benefits of early molar extraction in preventive dental care, reducing the likelihood of complex treatments later.
What should patients expect before a molar removal?
Knowing what’s coming can ease a lot of stress. Here’s what most patients can expect in the lead-up to their wisdom tooth procedure:
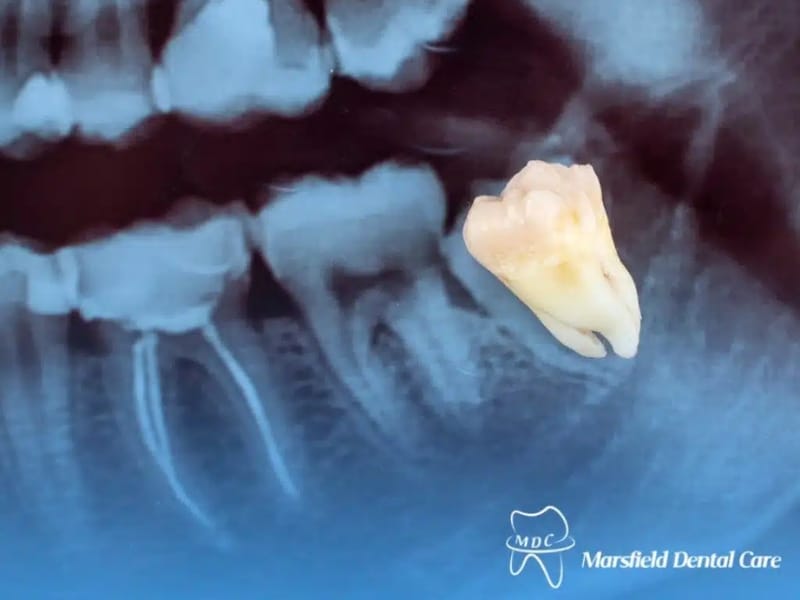
- Consultation and imaging: A panoramic X-ray helps the dentist understand tooth position and plan the best approach.
- Numbing and anaesthesia options: You’ll be offered a local anaesthetic, and sometimes sedation if anxiety is high.
- Procedure prep instructions: You may need to fast, arrange a lift home, or stop certain meds beforehand.
- Post-op care planning: Stock up on soft foods, ice packs, and pain relief ahead of time.
Here’s a quick comparison:
| Step | What to Expect |
| X-rays | Show tooth position and root structure |
| Anaesthesia | Numb pain may include sedation for comfort |
| Removal Method | Surgical or straightforward, depending on complexity |
| Recovery | Swelling, soreness, soft diet for 3–5 days |
Understanding the steps helps you go in calm and come out on track for smooth recovery.
Final thoughts
There’s no doubt wisdom teeth can stir up some serious trouble if left unchecked. But handled early, they don’t have to wreck your smile or undo years of dental work. If you’re weighing your options, it’s worth knowing how Marsfield Dental Care handles complex wisdom tooth cases — it offers clarity on what to expect and how to plan for a smoother experience.